By 2030, the World Health Organization (WHO) estimates a shortage of 18 million healthcare workers. Among them, half will be nurses, causing a global nursing shortage. And in the United States, those nurse job openings will soon outpace every other occupation there is—more than engineers, developers, accountants and yes, even physicians.
Because of an aging patient population, retiring workforce and nursing’s turnover, regional health systems are acutely affected by these trends—especially in areas where resources are tight and tenured nurses are as good as gold. In those environments especially, existing nurses can be stretched especially thin.
Can a clinical communication and collaboration (CC&C) tool help? If it’s deployed thoughtfully, then yes. But poorly executed technology can add stressors to a workforce already at risk of burnout. The challenge is to find a balance that works with workflows, rather than against them.
Here’s why that matters:
Labor Gaps and Burnout Are a Cycle
According to 2018 research from RNnetwork, nearly half of nurses consider leaving nursing entirely in pursuit of a new career—and many who stick around end up feeling overworked and underappreciated, which puts them at risk of leaving too.
It’s a cycle: Nursing shortages lead to burnout, and burnout leads to shortages, with lasting effects on patient safety and outcomes. But how can a health system break that cycle when they’re limited only to the staff they have—or that they can feasibly recruit for?
This is where efficiencies and workflow improvements can make a big difference. But just throwing technology at the problem won’t solve anything—and may make things worse. It must be the right approach.
Critical Nursing Shortage Capabilities
Nurses are understandably wary of desktop-based solutions that take them away from the bedside. But at the same rate, some mobile technologies have been found to markedly improve clinicians’ productivity and morale while removing friction and wasted costs. It’s a matter of deploying the right mobile strategy at the right time—starting with these essential features:
1. Real-Time Enterprise Directory
Think about the thousands of interactions you and your staff have over the course of a single shift. These interactions may be simple requests with yes/no answers, or they may be complex topics that require minutes of live discussion with people in different departments, buildings, or campuses.
A clinician may know they need to talk to a person in a particular role, but who? How do they know who is associated with the patients they need to discuss?
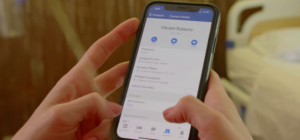
That’s why a real-time directory with a clear chain-of-command for every patient is critical. Within your organization’s CC&C platform, nurses should be able to see who’s on the patient’s care team; with a single tap, they should be able to call, text or video chat with them right away. (Systems that have deployed these tools have seen up to a 38 percent decrease in nurse steps during a 12-hour shift.)
2. Smarter Alerting
Alarm fatigue has damaging effects on clinicians and patients alike, nurses included. In response, healthcare systems are opting for smarter, more targeted alerting and nurse call through clinical communication platforms that can help reduce ambient noise on patient floors by 50 percent. An open integration environment coupled with alerting capabilities for things like telemetry, critical labs and nurse call all allow nurses to engage with their patients in quicker and easier ways.
Look for a clinical communication platform with customizable tones, automated escalation and the ability to respond directly within the alert pop-up—all of which can help nurses more portably collaborate with others using minimal screen time.
By putting a smartphone in the hands of nurses—directly at the point of care—healthcare organizations can see the biggest impact in response times to alerts and workflow escalations.
3. Integrated Mobile Tools
A key benefit of adopting a mobility solution is portability. Instead of being tied to a desktop computer for access to important information, clinical and ancillary staff can access relevant patient data, colleagues’ contact info and mission-critical applications wherever they are—directly from their phones. This becomes even more powerful when the applications on the smartphone actually integrate with each other in a cohesive ecosystem.
While basic collaborations, such as EHR integration, nurse call integration and telemetry are table stakes, it’s important that your organization’s communication platform provide open integrations with other vital systems.
With MH-CURE’s InterApp Launch Points™, for example, nurses can launch back and forth between medical reference materials, telemetry screens and other resources, so they can facilitate patient care collaboration without having to redundantly enter their login credentials.
Boost Nurse Satisfaction the Right Way
As nurses are asked to do more with less and the nursing shortage grows, expect mobile smartphone technology to play even more of an enabling role moving forward. Indeed, while no solution can replace the human element of nursing, the right tool can eliminate barriers and reduce burnout while making the most of the human talent you have.
Providing your nursing staff with the cutting-edge tools that they need, directly at the point of care, they can get back to doing what they love—caring for their patients. When clinicians are properly supported by technology, they won’t feel burdened by a nursing shortage.
After all, in this healthcare era, nurses are as good as gold. Are you doing all you can to make sure your colleagues are happy?